Healthcare
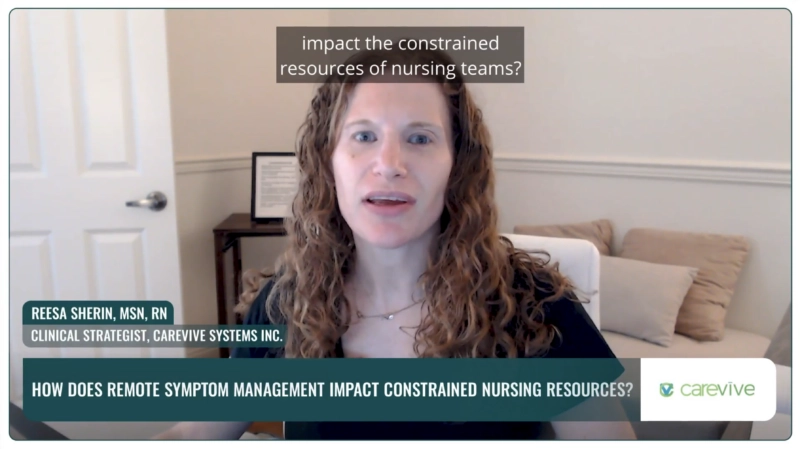
In the fast-paced world of healthcare, nursing teams play a vital role in supporting patients throughout their treatment journey. However, the sheer volume of incoming calls from patients, ranging from mild to severe symptoms, can overwhelm constrained nursing resources. This is where remote symptom monitoring and management steps in to make a difference. With Carevive’s…
Latest
Carevive
Was There a Positive Impact by Reporting Your Symptom Experience Remotely?
Facing a cancer diagnosis can be terrifying, leaving one with numerous unanswered questions and fears about the journey ahead. In a heartfelt account, a cancer patient shares how a wealth of information provided much-needed reassurance during this challenging time. The availability of comprehensive resources allowed the patient to find answers to her questions, easing her…
Carevive
Impact of Partnership with Carevive
Carrie Wines-Larch, a nurse navigator and survivorship coordinator, shares the challenges faced in the infusion clinic at the Cancer Center at Charleston Area Medical Center. Patients arriving unprepared for treatment due to scheduling difficulties and delayed referrals prompted the need for a solution. The implementation of Carevive’s clinic allowed for a pre-infusion check to ensure…
Carevive
Nurse Navigator Experience
In this insightful blog post, nurse navigators discuss the transformative impact of Carevive in their daily practice. Their main focus is educating patients about their treatment plans and identifying barriers to care, particularly psychosocial issues. The Carevive application has proven invaluable in fostering stronger relationships with patients, enabling weekly check-ins for real-time updates on their…
Carevive
How Does Carevive Align With FFS and Value – Based Reimbursement In The Future?
John Elliott from Carevive shares valuable insights gathered from recent conversations and on-site visits with partners and industry experts. The burning question on everyone’s mind is how Carevive aligns with the current fee-for-service reimbursement landscape and future value-based plans. In the current state, Carevive seamlessly aligns with chronic care management codes, benefiting patients with treatment…
Carevive
What Value Do You See Oncology Care Teams, Administrators and Patients Gaining Patient Experience Data?
Dr. Aaron Galaznik, Chief Scientific Officer of Carevive, introduces Carevive’s transformative platform, PROmpt, providing remote symptom monitoring and patient quality of life measurement during cancer treatment. Carevive’s smart data combines routinely assessed patient-reported outcomes with EMR-derived clinical data, ensuring a scalable and actionable approach to bring the patient perspective into cancer treatment. Published studies and…
Carevive
EOM Acceptance: What’s Next?
John Elliott from Carevive extends warm congratulations to oncology sites, cancer centers, and programs that have applied for the Enhancing Oncology Model (EOM). CMS has started sending acceptance letters, and it’s time to gear up for what’s next. Step one is to acknowledge the acceptance confirmation to ensure a smooth setup for the July start…
Latest
Latest Articles Healthcare
Survey Ready Every Day: Why It’s Not Just a Once-a-Year Activity
Unannounced surveys are no longer the exception in healthcare—they’re the norm. Accrediting bodies increasingly expect sterile processing departments (SPDs) to demonstrate consistent compliance, real-time documentation, and reliable adherence to manufacturers’ instructions for use on any given day, not just during audit season. Joint Commission survey data continue to show that high-level disinfection and sterilization practices…
How Predictive AI Is Helping Hospitals Anticipate Admissions and Optimize Emergency Department Throughput
Emergency departments across the U.S. are under unprecedented strain, with overcrowding, staffing shortages, and inpatient bed constraints converging into a throughput crisis. The American Hospital Association reports that hospital capacity and workforce growth have lagged, intensifying delays from arrival to disposition. At the same time, advances in artificial intelligence are moving from experimental to operational—raising…
Caregiver Engagement Is the Missing Link in Dementia Care: Why Empowering Families Drives Better Outcomes and Lower Costs
Dementia is becoming one of healthcare’s most difficult problems to ignore. As the population ages, more families are finding themselves responsible for loved ones who can no longer manage their own care, communicate symptoms clearly, or navigate the healthcare system. Research shows that people living with dementia are hospitalized far more often than those without it—even…
The Silent Foundation of Patient Safety: Why Water Quality Matters in Sterile Processing
In healthcare, patient safety and operational efficiency often depend on invisible systems working perfectly in the background. One of those systems—water quality—has quietly become a defining factor in sterile processing success. With new standards such as AAMI ST108 setting stricter expectations, hospitals, and SPDs (Sterile Processing Departments) are rethinking how they monitor, manage, and measure…
The SPD Hack Playbook: Streamlining Sterile Processing with Smart Tech and Team Buy-In
Sterile Processing Departments (SPDs) are the unsung backbone of surgical care — ensuring every instrument, tray, and tool is safe, sterile, and ready when needed. Yet, despite their vital role, SPD workflows often rely on manual processes and underrecognized best practices. As healthcare systems push for greater efficiency and staff well-being, SPD managers are turning…
Hot Takes on Rural Healthcare: Lessons from the Frontlines of a System in Decline
Across America, rural hospitals are facing an existential crisis. From physician burnout and recruitment struggles to malpractice insurance woes and shrinking OB units, the challenges facing small health systems are multiplying. According to the National Rural Health Association, roughly 190 rural hospitals have closed down or discontinued inpatient care since 2010 — and many more…
The Open Road to Reform: Why Healthcare Needs Disruption, Innovation, and the Return of Real Competition
The U.S. healthcare system is at a crossroads — facing rising costs, limited competition, and a widening gap between innovation and accessibility. According to projections from the Centers for Medicare & Medicaid Services (CMS), national health spending is expected to grow faster than the overall economy over the next decade — about 5.8% per year…
The Future of RCM: Leveraging AI, Automation, and Human-Centered Design to Transform Patient Financial Care
Hospitals today are juggling tighter budgets, shifting regulations, and increasingly savvy patients—all while trying to keep financial operations running smoothly. That pressure has made the revenue cycle a powerful lever for innovation. The spread of artificial intelligence (AI) and automation is no longer experimental; it’s reshaping how health systems manage billing, reimbursement, and patient engagement….
Lasting Success in Healthcare Depends on Human Understanding: Why the Most Resilient Revenue Cycles Are Built on Empathy, Not Algorithms
Hospitals today are fighting a two-front battle — one against increasingly sophisticated payers armed with automation and AI, and another to meet patients’ rising expectations for clarity and convenience. A recent joint study by Knowtion Health and the Healthcare Financial Management Association found that nearly one in two revenue cycle executives now identify payer denials…
Latest Healthcare Podcasts
The Legacy of Dr. G. Duncan Finlay – Episode 6
The Rothman Index, developed by Dr. Michael Rothman and his brother Steven, is a pioneering patient acuity score designed to help clinicians recognize patient deterioration earlier and more clearly. Presented as an easily understood, color-coded graph that updates in real time, the Index displays upward and downward trends in patient condition at a glance—transforming…
The Origin Story of the Rothman Index – Episode 5
Hospitals collect enormous amounts of clinical data, yet preventable patient decline remains a persistent challenge. Over the past two decades, hospitals have invested heavily in early warning scores and rapid response infrastructure, but translating data into timely, meaningful action has proven difficult. As clinicians contend with alert fatigue and increasing documentation burden, a more…
My Mother and the Story of the Genesis of the Rothman Index – Episode 4
Healthcare generates enormous volumes of clinical data, yet making sense of that information in real time remains a challenge. Subtle changes in vitals, labs, and nursing assessments often precede serious events, but when that information is fragmented across the medical record, emerging risks can go unnoticed. The central challenge facing hospitals today is not…
Career Development for Global Pediatric Nurses
The Care Anywhere podcast is spotlighting a new global partnership designed to strengthen pediatric nursing education and recognition worldwide. In this episode, host Lea Sims sits down with leaders from TruMerit and the National Association of Pediatric Nurse Practitioners (NAPNAP) to unpack a new pediatric nursing micro-credential pathway launching in 2026, and why it…
How Simulation-Based Education Is Transforming Healthcare Leadership and Decision-Making Worldwide
As healthcare systems worldwide face rising costs, workforce shortages, and increasing pressure to balance quality with financial sustainability, traditional classroom-based management education is struggling to keep pace. According to the World Economic Forum, healthcare spending now accounts for nearly 10% of global GDP, making leadership decision-making more consequential—and more complex—than ever. At the same…
Inside ERISA Denials: Why Employers May Be the Real Decision-Makers Behind Your Insurance Card
Insurance denials aren’t new, but they’re hitting a breaking point right now. As prior authorizations surge and patients face longer delays for everything from imaging to specialty drugs, more providers are realizing that the “payer” on the card often isn’t the one truly holding the reins. A growing share of Americans are covered…
Patient Care and Orthopedic Innovation in the Age of AI: Why Human Skill Still Outweighs Robotics
The rise of artificial intelligence in medicine is reshaping how orthopedic surgeons diagnose, plan, and deliver care. From robotics in the operating room to AI-driven diagnostics and bone segmentation tools, orthopedic innovation is advancing rapidly. Yet, adoption in everyday surgical practice has been more measured. For example, in 2022, robot-assisted technology accounted for…
Leading Through Change: Dr. Kevin Stevenson on Workforce, Innovation, and the Future of Healthcare
Healthcare is at a critical turning point, where staffing pressures, shrinking reimbursements, and rising patient expectations are reshaping the future of healthcare. According to the AACN Nursing Workforce Fact Sheet, the federal government projects more than 203,000 new registered nurse positions will be created annually from 2021 to 2031, reflecting high demand from an…
Transformation Without Disruption: How Access Healthcare Is Rewiring the Revenue Cycle with Agentic AI
Hospitals are juggling shrinking margins and rising costs while denial volumes remain stubbornly high. In the revenue cycle alone, hundreds of billions are lost annually to preventable errors and inefficiencies—in fact, Access Healthcare CEO Shaji Ravi cites more than $250 billion wasted each year. Meanwhile, payers have accelerated their use of AI to adjudicate…
Latest Videos Healthcare
What the Future Looks Like if We Get It Right
As the Patient Monitoring series concludes, the conversation shifts from today’s challenges to tomorrow’s possibilities. This final episode of the five-part Health and Life Sciences at the Edge series looks ahead to what healthcare could become if patient monitoring gets it right. Intel’s Kaeli Tully is joined by Sudha Yellapantula, Senior Researcher at Medical…
Why We Show Up for Care
Episode 4 of The Future of Patient Monitoring takes a step back from infrastructure and innovation to explore something deeper: the people behind the technology—and what they’ve learned through years of building smarter systems. Part of the Health and Life Sciences at the Edge podcast series, this conversation is led by Intel’s Kaeli Tully,…
Career Development for Global Pediatric Nurses
The Care Anywhere podcast is spotlighting a new global partnership designed to strengthen pediatric nursing education and recognition worldwide. In this episode, host Lea Sims sits down with leaders from TruMerit and the National Association of Pediatric Nurse Practitioners (NAPNAP) to unpack a new pediatric nursing micro-credential pathway launching in 2026, and why it…
The Hidden Roadblocks to Smarter Hospitals
As hospitals look to improve outcomes with faster, more informed decisions, infrastructure limitations remain a major hurdle. This episode—part two of a five-part Health and Life Sciences at the Edge series exploring The Future of Patient Monitoring—dives into what’s holding back smarter, more connected care. Intel’s Andrew Lamkin, AI Solutions Architect, and Bikram Day,…
ROI Case Study
Denials are no longer a slow leak in the revenue cycle—they’re a fast-moving, rule-shifting game controlled by payers, and hospitals that don’t model denial patterns in real time end up budgeting around losses they could have prevented. PayerWatch’s four-digit, client-verified ROI in 2024 shows what happens when a hospital stops reacting claim by…
Clip 2 – Fighting for Coverage: One Patient’s Story
Health insurers love to advertise themselves as guardians of care, but the real story often begins when a patient’s life no longer fits neatly into a spreadsheet. In oncology especially, “coverage” isn’t a bureaucratic checkbox—it’s the fragile bridge between a treatment that finally works and a relapse that can undo years of grit…
The Sustainability of the Healthcare System
The sustainability of the healthcare system won’t be secured by another round of cost-cutting or clever benefit design alone, but by a hard cultural pivot toward alignment: payers, providers, employers, and patient advocates pulling on the same rope instead of grading each other on different exams. Right now we’ve built a maze that…
Allow Doctors to Provide Care Without Making Patients Fight the Insurance System
Patients shouldn’t have to become their own case managers just to access a hip replacement, transplant, or any other life-changing procedure; the moment they’re pushed into a paperwork fight, the system has already shifted its burden onto the sick. In a functional healthcare model, clinicians and their teams handle the insurer negotiations behind…
The Impact of Physician Advisors on Hospital Revenue and Patient Advocacy in a Payer-First Era
Physician advisors are becoming the quiet linchpin of hospital resilience in a reimbursement environment where insurers increasingly treat care like a spreadsheet exercise. As payers tighten criteria and automate denials, the gap between clinical reality and business logic widens—and without a skilled physician advisor (and a disciplined appeals pathway), health systems risk watching…